Most of the education we receive—whether through conferences, lectures, fellowships, or even mentorship programs—shares a common limitation: it teaches us principles and even supplements them with case studies, but it rarely offers real-time support for the unique challenges a new patient brings to the table. When you’re face-to-face with a patient whose clinical picture is unlike any you’ve seen before, you need more than theory. You need a system that can guide you at the point of care, in real time, ensuring you uphold the high standards your practice is known for.
As a functional or precision medicine doctor, you’ve likely spent years perfecting your craft. You’ve poured time and resources into postgraduate education, attended dozens (maybe hundreds) of conferences, and learned the intricacies of personalized medicine to reverse chronic illness. Through trial, error, and dedication, your clinic has thrived.
Now, you’re at the point where demand is higher than you alone can handle. Patients are seeking out your expertise in droves—and it’s time to hire a second practitioner.
But here’s the challenge: the “Second Practitioner Problem.” The knowledge gap between your wealth of experience and what a new team member brings to the table can be huge. If this new practitioner isn’t equipped with the right training, systems, or mentorship, you risk seeing your clinic’s hard-earned care standards slip. The result? Disappointed patients, extra stress on you, and a potential dip in reputation.
Below are three approaches real clinics are using to tackle the Second Practitioner Problem, with differing levels of success:
1. The Residency Approach (à la Parsley Health)
Parsley Health, founded by Dr. Robin Berzin, recognized early on that few incoming doctors possess the deep, practical skills required to deliver high-level functional medicine. Their solution was to build an internal “residency” model—a structured, in-depth training program that immerses new hires in Parsley’s standard of care.
How It Works:
Practitioners follow a strict onboarding curriculum, shadow senior doctors, and regularly review cases. This ensures every new team member can confidently deliver a uniform level of care.Upside:
Parsley Health has grown to about 50 doctors, many of whom successfully deliver the same high standards established by Dr. Berzin.Downside:
Building a residency program is a resource-intensive feat. Most independent clinics don’t have the infrastructure or capital to replicate this model at a small scale.
2. The Standard Package Model (Freedom Practice Coaching)
Freedom Practice Coaching (FPC) promotes a strategy where each patient receives a standardized, well-defined care journey—at least for the first few months.
How It Works:
New hires simply apply the same 60-day gut and detox program, delivering a consistent experience and baseline education to each patient. Individualization can happen once those foundational weeks have passed.Upside:
The practice can onboard a new doctor relatively quickly: everyone follows a proven template. During the early phase, your clinic maintains consistent quality for all patients.Downside:
By giving every patient the same protocol, you risk diluting the truly personalized aspects of functional medicine. Some patients may feel like they’re on a “one-size-fits-all” track, rather than receiving customized care.
3. The Next-Gen Clinical Mentorship (TruNeura)
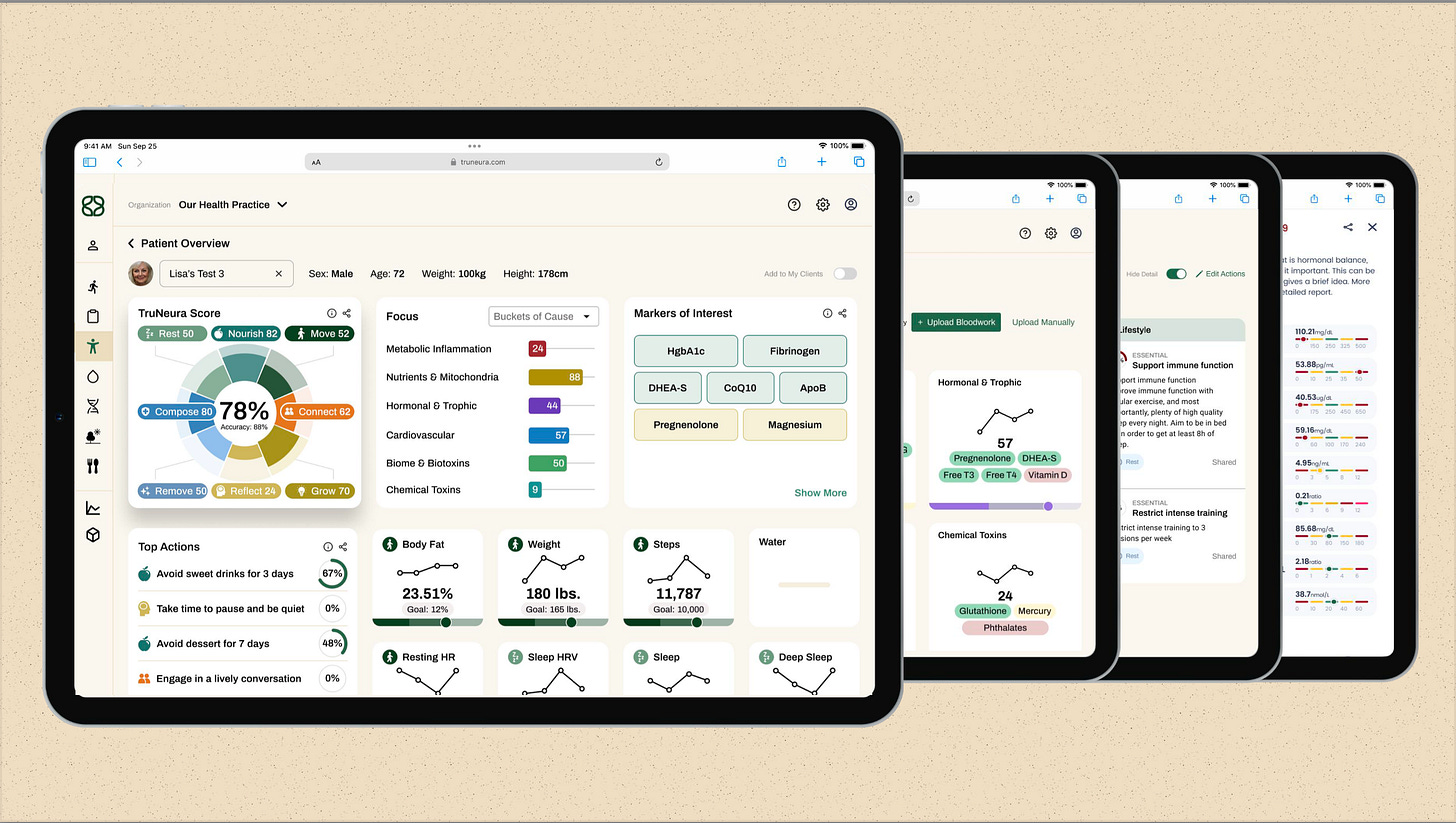
A more technology-driven method has emerged: using an AI-enabled, data-centric platform that effectively acts as a clinical mentor to new practitioners.
How It Works:
With TruNeura, doctors can score patient labs, organize root-cause factors (like metabolic inflammation or toxins), and generate recommended next steps. This ensures that even a less-experienced provider has the guidance to match the care standards of a veteran doctor. The system is advanced enough to handle intricate protocols—especially for specialized niches such as brain health.Upside:
TruNeura offloads a significant chunk of the knowledge gap. It’s like having a veteran mentor constantly reviewing cases, offering reminders, and making suggestions. Clinics can even use this system to roll out a new Brain Health Membership, with the newer practitioner focusing on that specialty while the technology ensures consistent outcomes.Downside:
A robust software solution still requires training, infrastructure, and staff buy-in. However, compared to building an in-house residency or forcing a uniform care path for everyone, a well-tuned tech platform can offer a more nuanced, truly personalized experience.
Bridging the Gap and Growing Your Practice
The Second Practitioner Problem doesn’t have to hold your practice back. Each of these strategies aims to ensure that as you grow, you don’t sacrifice clinical excellence. TruNeura, in particular, meets the need for individualized care while helping newer deliver the same quality you’ve achieved through years of study—without burdening you to train them every step of the way.
Ready to see how technology can supercharge your new practitioner’s skills—while giving your patients the personalized protocols they expect?
Click here to download our free guide and discover how the right systems, frameworks, and AI-backed mentorship can help you bring on a second practitioner without compromising the care you’re renowned for. Here’s to scaling your impact, boosting revenue, and—above all—delivering life-changing results for every patient who walks through your door!