Dr. Bredesen vs. The New York Times: Whose Model Is More Predictive?
The battle for the truth about brain health hits the mainstream
This week, The New York Times published yet another example of what has become a familiar genre: the wellness hit piece. This time, the target was Dr. Dale Bredesen, a neurologist who has spent the last decade challenging the status quo in cognitive decline care with a bold and hopeful question: Can Alzheimer’s be reversed?
The article, filled with skepticism, half-contexts, and the usual subtle character digs, does what so many articles like this have done: punch down at those daring to rethink chronic disease, especially when they sit at the uncomfortable intersection of medicine and wellness. It paints Bredesen as something close to a charlatan, sidestepping decades of his published research, ignoring the deep logic of his model, and glossing over the mounting evidence that precision medicine works.
Frankly, it’s borderline libelous. But more importantly, it forces us to ask a better question:
Whose model is more predictive?
Bredesen’s precision model of Alzheimer’s? Or conventional neurology’s failed drug-first paradigm?
The Scientific Trail: From Case Series to Controlled Trial
Let’s start with what science actually looks like.
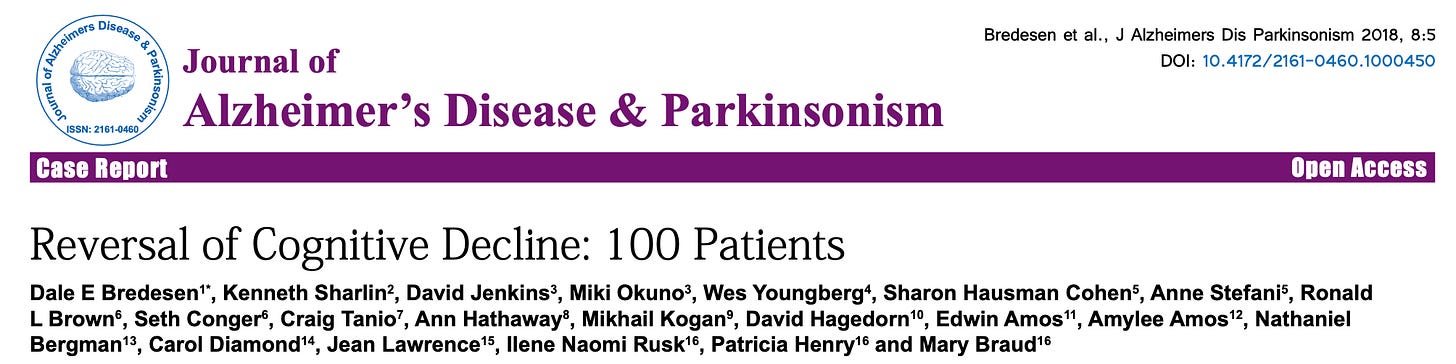
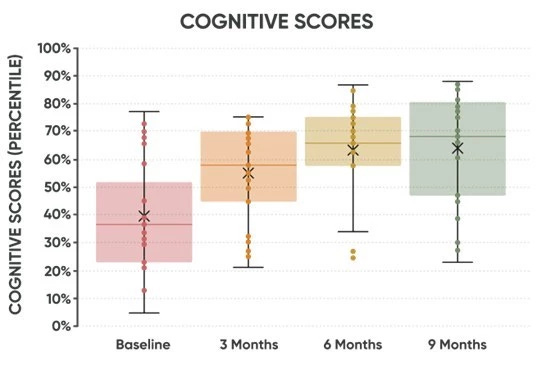
When Dr. Bredesen first began reversing cognitive decline in patients, he did what any careful clinician does: he published a case series. Not anecdotes—documented clinical outcomes. A series of 100 patients who showed improvements on objective cognitive scores. That’s how paradigm shifts begin.
Then came the 2022 study in the Journal of Alzheimer’s Disease, comparing his precision protocol to the current standard of care. The results weren’t subtle—they were substantial. Patients following Bredesen’s multifactorial approach got better, while those in the standard model continued to decline. We have the graphs. We have the data.
Now, he’s running the first randomized, placebo-controlled trial of the Bredesen protocol. You can follow the progress at DementiaReversalTrial.com.
One of the key sites for that trial is led by Dr. Kristine Burke, founder of TruNeura, whose patients have seen an average MoCA score improvement of 4.2 points—a number virtually unheard of in traditional neurology.
And yet, The New York Times felt comfortable writing him off as fringe.
A Model That Predicts—and Reflects Reality
Let’s talk about predictions. In general - those who can predict the future have a more accurate model of reality.
The core of Bredesen’s model is simple: Alzheimer’s and cognitive decline are multifactorial. He identifies multiple “types” or patterns of decline—metabolic, toxic, vascular, infectious, hormonal, traumatic—and outlines a precision approach to addressing them.
Sound radical?
Not anymore.
Just this month, a study made headlines showing that living near golf courses increases Parkinson’s risk—something that seems baffling to conventional neurology. But not to Dr. Bredesen and the precision medicine doctors that follow him or have been mentored by him.
The timing couldn’t be more apt as this week’s Make America Health Again Commission released it’s findings and even though that was related to children the same themes emerge when it comes to the root causes of chronic illness
Environmental toxins
Overmedication
Food environment and metabolic health
Overuse of technology
All of these are predicted and communicated as part of Dr. Bredesen’s work.
And the New York Times should have known better, only 5 months ago it was accurately documenting the state of science in Alzheimer’s. The only thing worse than overmedication and polypharmacy is using drugs that don’t work or have studies with unhelpful end points.
Terry Wahls and the Pattern of Pushback
And let’s not forget Dr. Terry Wahls, another pioneer who was initially dismissed and banned from MS conferences after she began sharing her story of reversing her own multiple sclerosis using a nutrient-dense, lifestyle-based protocol. Now, her methods are being taught inside the VA system, and her results are replicated in study after study.
It’s the same pattern we see with Dr. Bredesen:
Radical idea that reflects systems biology
Early success stories
Media and medical system pushback
Slow, undeniable accumulation of evidence
Eventual mainstream acceptance—decades later
We’ve seen this movie before. But this time, we don’t have decades to wait. Cognitive decline is rising faster than our medical system can respond. And we already have a model that works.
Check out Dr Bredesen’s rebuttal to the New York Times “Setting the Record Straight. Yes, cognitive decline can be reversed”
The Real Story: Hope, Empowerment, and Action
Dr. Bredesen’s model is empowering. It tells patients: you’re not broken, and you’re not helpless. It encourages doctors to move beyond Rx and explore sleep, toxins, infections, hormones, community, and purpose. It puts the patient in the center of a supportive system—a model that must include personalization, participation, and pattern recognition.
Is that messy? Sure. It doesn’t reduce to a single biomarker or a single pill. But it reflects the reality of human physiology, not the constraints of reimbursement model or drug first paradigm.
So... Whose Model Should You Bet On?
On one side:
A neurologic model that still doesn’t know where Alzheimer’s comes from
Failed drug after failed drug m
A pipeline of expensive “breakthroughs” that don’t reverse decline
On the other:
A model that predicted toxins, metabolism, and inflammation before they were trendy
Real-world case studies
A published trial
A growing community of clinicians seeing consistent outcomes
We’ll leave it to you to decide.
But over here, we know which side we’re supporting.







James, such a thoughtful and well-written rebuttal. As someone who teaches the Bredesen Protocol I wholeheartedly agree with your assessment and feel that Dr Bredesen should be revered for his pioneering work. If they understood systems biology, they would not be debating this. Makes me wonder why is the system that has been unable to offer anything successful for Alzheimer’s patients so threatened by these hopeful results? Thank you for writing this.
Thank YOU for defending Dr. Bredesen! The BIAS in the NY Times article is particularly obvious when they mention that he has chosen to not renew his medical license because he had lost faith in the conventional medical model...and thus, the NY Times chose to refer to him as "MR. Bredesen." Just because a person doesn't renew his or her medical license doesn't mean that they do not have an MD degree...they simply don't have a license to practice medicine.
It is also interesting how this article chose to totally ignore the serious fraud that has recently taken place in Alzheimer's research, about which the NY Times has previously reported: https://www.nytimes.com/2025/01/24/opinion/alzheimers-fraud-cure.html
And of course, all of this biases reporting becomes evidence in the latter part of the article where the writer choses to attack RFK and new efforts to Make America Healthy Again. Clearly, the NY Times does NOT want to make America healthy again! Sad, but true.
In the past, I had a lot of respect for the NY Times...but they have totally lost my respect over the past decade.